An overview of how Revvity solutions and associated technologies support the application, optimization, and refinement of gene therapies.
The overarching goal of gene therapy is to modify gene expression to treat disease.[1] Researchers first began to think about how modification could be achieved as the first molecular biology techniques were developed in the 1970s.[2-4] These cutting-edge therapies deliver functional genetic payloads, which is very different from administering a known quantity of a drug. Providing a precise gene dose to the affected cells in the patient’s body is paramount to safety and efficacy and requires accurate quantification and thorough preclinical testing. Furthermore, moving from the bench to the clinic requires extensive immunogenicity testing, as every component of a gene therapy product from the vector to cargo to therapeutic protein can elicit an immune response. Gene therapy is regulated by the U.S. Food and Drug Administrations’ Center for Biologic Evaluation and Research.[5-11]
There are three main approaches to gene therapy:
- Replacing the mutated gene with a normal copy
- Inactivating the mutated gene to prevent it from causing more harm
- Introducing a new gene to treat a disease
Gene therapy is accomplished through in vivo or ex vivo therapy
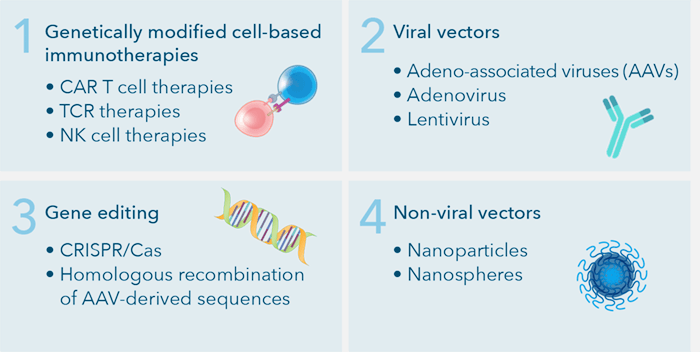
Broadly speaking, gene therapy is ex vivo or in vivo.[12, 13] Ex vivo gene therapy involves harvesting cells from the patient, modifying the DNA, expanding the modified cells, and infusing them back into the patient. In in vivo gene therapy, the targeted cells are altered inside the body and the gene therapy is administered directly to the patient. This approach is more technically challenging because it requires targeted delivery of the payload to the affected cells and or tissues, where the gene must be effectively expressed. Gene therapy utilizes four broad categories to combat these issues: genetically modified cell-based immunotherapies, viral vectors, non-viral vectors, and gene editing.[17-20]
Of the four main types of gene therapies, viral vectors are incredibly efficient at transfecting or transducing host cells. For this reason, up until 2017, ~70% of the 3000+ clinical trials conducted employed viral vectors.[21]
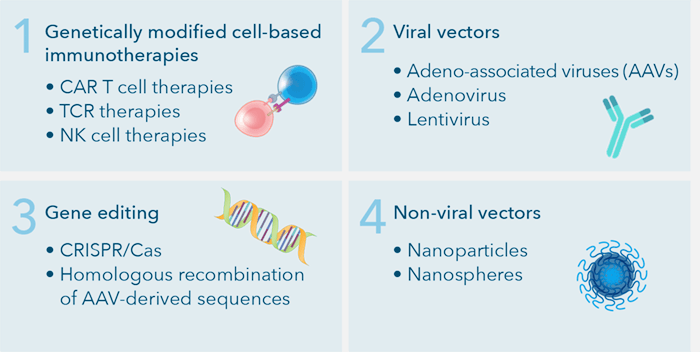
Four main types of gene therapy: genetically modified cell-based immunotherapies, viral vectors, gene editing, and non-viral vectors.
In general, viral vector-based gene therapy development follows several relatively complex workflows.[22] First, gene therapy products are unique in that they are produced in mammalian cells, so it is critical to select and isolate suitable target cells during preclinical research and development. Next, the appropriate vectors are selected based on the following considerations:
- DNA load capacity
- Transduction efficiency
- Cell tropism
- Target cell mitotic status
- Geno-/cytotoxicity
- Limited-to-no immune response in humans
Subsequently, assay development is required to determine the transduction efficiency to ensure the proper gene is transduced into the selected cell types. Finally, due to safety concerns, researchers are required to screen vector antibodies in patient sera to test for transduction inhibition.
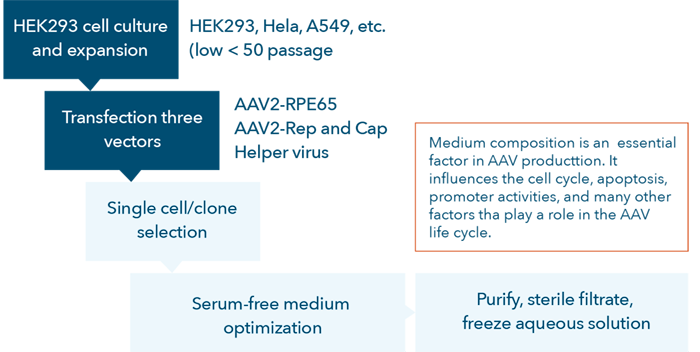
AAV vector development process flow chart.
Current technologies for gene therapy research and development
Many technologies and methodologies are employed for gene therapy research and development such as PCR, cell-based assays, LC-MS, flow cytometry, ELISpot, etc. Cell-based assays are one of the most commonly used methodologies for gene therapy development in academia and industry.
These existing technologies also face various challenges:
- Sensitivity
- Robustness
- Sample availability for method development and validation
- Selectively
- Sample availability for all analyses required
- Sample matrix type
- Sample stability
Viral vector-based gene therapy research can present some challenges when developing and optimizing cell-based assays:
- Designing effective vectors
- Increasing transduction efficiency
- Optimizing culture conditions
- Banking cells
- Measuring gene expression
- Scaling up production
- Effective delivery to cells in vivo (due to pre-existing neutralizing antibodies)
Image cytometry assays improve speed and efficiency for cell counting and cell-based assays
Revvity’s image cytometry and automated cell counting systems support three important aspects of viral vector-based gene therapy research and development. First, they provide rapid, user-friendly solutions for cell counting, measurement of transduction efficiency, proliferation, viability, cytotoxicity, and apoptosis as well as other biological phenomena to support researchers developing new gene therapies. Additionally, image cytometry methods can be used to test patient samples for pre-existing antibodies that may prevent the therapy from being effective and to help monitor immune responses during treatment.
Quality control to develop high-quality cell cultures:
- Rapid cell counting
- Accurate assessment of proliferation and viability
- Cell culture condition optimization
- Cloning selection and verification
Selecting and fine-tuning an appropriate AAV vector:
- Simultaneously assess transduction efficiencies and expression level
Developing screening assays to identify pre-existing antibodies in patients:
- Screen patients for vector-neutralizing antibodies
- Cell-based in vitro neutralization assays
Improve research efficiency and quality of product development
Cell-based assays are highly important for gene therapy research and development. Image cytometry and automated cell counting systems are utilized to optimize cell-based assays.
Cell quality:
- Cell count, viability, and apoptosis by caspase 3/7 or Annexin V can confirm the quality of the cells before experimentation (Cellometer Spectrum, Auto 2000 or K2 cell counters)
- A large number of samples can be quickly assessed (Cellaca MX high-throughput cell counter)
- Advanced cell-based assays such as cell proliferation, cell cycle, apoptosis, and senescence can be performed in 96- or 384-well plates (Celigo image cytometer)
Cell culture condition optimization:
- Media and reagent optimization can be measured by assessing cell proliferation within wells in 6- to 96-well plates (Celigo image cytometer)
- High-throughput cell counting is needed before seeding cells to assessing multiple conditions (Cellaca MX high-throughput cell counter)
Transduction and expression efficiency:
- Transduction efficiencies can be measured by direct cell counting of total and fluorescent-positive cells (Cellometer Spectrum and Celigo image cytometers)
- Expression level can be determined by measuring fluorescent intensities in genetically modified cells (Cellometer Spectrum and Celigo image cytometers)
Single-cell clone verification:
- Whole-well imaging is required to ensure single-cell monoclonality and can be quickly determined through brightfield colony outgrowth or directly using fluorescence (Celigo image cytometer)
Screen pre-existing antibody to AAV in sera
An antibody or serum-based neutralization assay:
- Pre-existing immunity to viral vectors can lead to neutralization and requires a cell-based in vitro transduction inhibition assay for screening (Celigo image cytometer)
Monitor immune responses
Humoral immune response by ELISAs of serum levels for vector:
- Requires accurate PBMC enumeration for ELISA analysis (Cellaca MX high-throughput cell counter)
T cell immune responses by ELISpot IFN-γ test:
- Requires accurate PBMC enumeration for ELISpot analysis (Cellaca MX high-throughput cell counter)
References
- asgct.org/education/more-resources/gene-and-cell-therapy-faqs
- Friedmann T, Roblin R. Gene therapy for human genetic disease. Science. 1972;175:959-955.
- Friedmann T. A brief history of gene therapy. Nat Genet. 1992;2:93-98.
- exploregenetherapy.com/history-of-gene-replacement-therapy
- U.S. FDA. 2020. Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs). Available at: fda.gov/regulatory-information/search-fda-guidance-documents/chemistry-manufacturing-and-control-cmc-information-human-gene-therapy-investigational-new-drug
- U.S. FDA. 2020. Human Gene Therapy for Hemophilia. Available at: fda.gov/regulatory-information/search-fda-guidance-documents/human-gene-therapy-hemophilia
- U.S. FDA. 2020. Human Gene Therapy for Rare Diseases. Available at: fda.gov/regulatory-information/search-fda-guidance-documents/human-gene-therapy-rare-diseases
- U.S. FDA. 2020. Human Gene Therapy for Retinal Diseases. Available at: fda.gov/regulatory-information/search-fda-guidance-documents/human-gene-therapy-retinal-disorders
- U.S. FDA. 2020. Interpreting Sameness of Gene Therapy Products Under the Orphan Drug Regulations. Available at: fda.gov/regulatory-information/search-fda-guidance-documents/interpreting-sameness-gene-therapy-products-under-orphan-drug-regulations
- U.S. FDA. 2020. Long Term Follow-up After Administration of Human Gene Therapy Products. Available at: fda.gov/regulatory-information/search-fda-guidance-documents/long-term-follow-after-administration-human-gene-therapy-products
- U.S. FDA. 2020. Testing of Retroviral Vector-Based Human Gene Therapy Products for Replication Competent Retrovirus During Product Manufacture and Patient Follow-up. Available at: fda.gov/regulatory-information/search-fda-guidance-documents/testing-retroviral-vector-based-human-gene-therapy-products-replication-competent-retrovirus-during
- Goswami R, Subramanian G, Silayeva L, et al. Gene therapy leaves a vicious cycle. Front Oncol. 2019;9:297. doi: 10.3389/fonc.2019.00297
- Van Haasteren J, Li J, Scheideler OJ, et al. The delivery challenge: fulfilling the promise of therapeutic genome editing. Nat Biotechnol. 2020. doi: 10.1038/s41587-020-0565-5
- Zheng PP, Kros JM, Li J. Approved CAR T cell therapies: ice bucket challenges on glaring safety risk and long-term impacts. Drug Dis Today. 2018;23:1175-1182. doi: 10.1016/j.drudis.2018.02.012
- Feins S, Kong W, Williams EF, et al. An introduction to chimeric antigen receptor (CAR) T-cell immunotherapy for human cancer. Am J Hematol. 2019;94:S3-S9. doi: 10.1002/ajh.25418
- Mohanty R, Chowdhury CR, Arega S, et al. CAR T cell therapy: A new era for cancer treatment. Oncol Rep. 2019;42:2183-2195. doi: 10.3892/or.2019.7335
- Senís E, Farouros C, Große S, et al. CRISPR/Cas9-mediated genome engineering: an adeno-associated viral (AAV) vector toolbox. Biotechnol J. 2014;9:1402-1412. doi: 10.1002/biot.201400046
- Hidai C, Kitano H. Nonviral gene therapy for cancer: a review. Diseases. 2018;6:57. doi: 10.3390/diseases6030057
- Milone MC, O’Doherty U. Clinical use of lentiviral vectors. Leukemia. 2018;32:1529-1541.
- Rosenblum D, Gutkin A, Dammes N, et al. Progress and challenges towards CRISPR/Cas clinical translation. Adv Drug Deliv Rev. 2020. doi: 10.1016/j.addr.2020.07.004
- Lundstrom K. Viral vectors in gene therapy. Diseases. 2018;6:42.
- Garcia-Perez L, Ordas A, Canté-Barrett K, et al. Preclinical development of autologous hematopoietic stem cell-based gene therapy for immune deficiencies: a journey from mouse cage to bed side. Pharmaceutics. 2020;12:549. doi: 10.3390/pharmaceutics12060659
For research use only. Not for use in diagnostic procedures.




























