What is PGT-M?
Monogenic disorders are caused by mutations in a single gene. Couples who are identified as carriers of known monogenic condition have a risk of passing it on to their offspring, leading to a wide range of health issues for the newborn. The overall frequency of carrier couples ranges from 1% to 2% but there is a lot of variation depending on the specific disorder and population considered. For example, cystic fibrosis, a common disorder among non-Hispanic White people of Northern European descent, has a carrier frequency of ~4%.
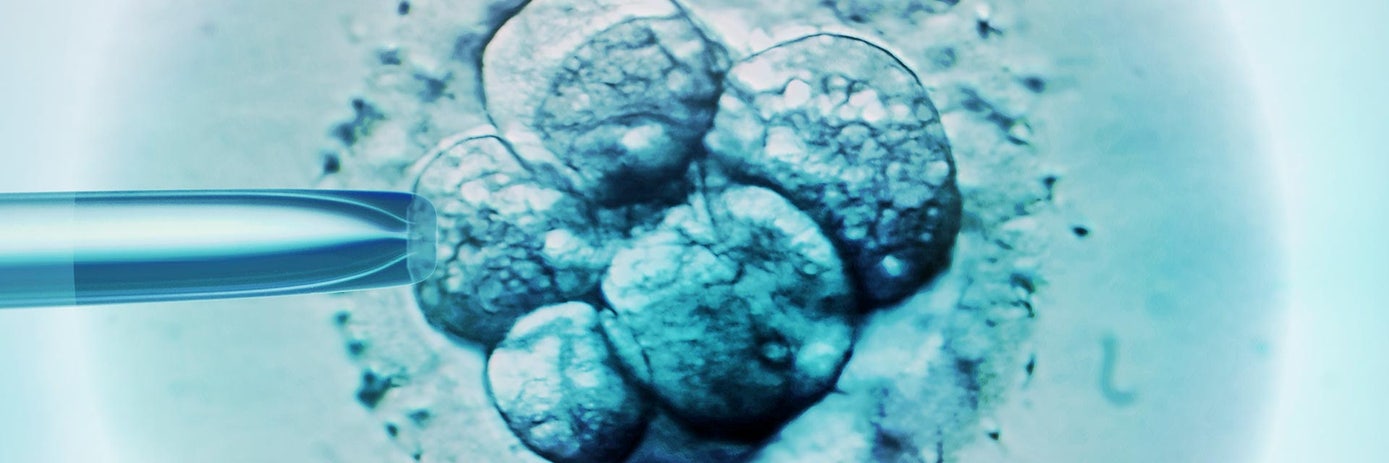
Preimplantation Genetic Testing for Monogenic Disorders (PGT-M) can reduce this risk. PGT-M involves the biopsy of a single or few cells from in vitro fertilized embryos and testing of the biopsied samples for known mutations inherited from one or both parents. This is followed by selective transfer of embryos unaffected for the conditions under study. The results of recent study of a cohort of couples affected by hereditary nephropathy supports PGT-M as an effective means of preventing intergenerational inheritance of monogenic disorders.
While PGT-M is a type of Preimplantation Genetic Testing (PGT), it differs significantly from other PGT techniques, most notably PGT-A (Preimplantation Genetic Testing for Aneuploidy). The three main types of PGT currently used in assisted reproduction centers are described below.
| Type | Focus | Indication |
|---|---|---|
| PGT-M | Targets specific single-gene disorders, with the goal of identifying embryos free of the inherited mutation | For couples with a family history of a mongenic disorder or those identified as carriers through genetic screening |
| PGT-A | Screens for chromosomal abnormalities such as extra or missing chromosomes which can lead to conditions like Down syndrome. Aims to identify embryos with the correct number of chromosomes to improve IVF success rates and reduce miscarriage risk | Often recommended for women over 35, those with a history of recurrent miscarriages, previous IVF failures or known chromosomal abnormalities in one of both parents |
| PGT-SR | Identifies structural chromosomal rearrangements, such as translocations or inversions, which can affect embryo viability. | Suggested for couples where one partner has a known structural chromosomal rearrangement, which can lead to infertility or recurrent pregnancy loss |
The Role of PGT-M in Detecting Monogenic Disorders
PGT-M can in theory be offered for any monogenic disorders for which the disease-causing loci have been unequivocally identified. These loci are nuclear or mitochondrial and involve (likely) pathogenic genetic variant(s). In practice the provision of PGT-M is regulated at each country and applicable conditions may differ across different regions. Some countries have quite restrictive legislation regarding acceptable conditions for testing while others are more liberal.
The more frequent indications for which PGT-M are currently applied are cystic fibrosis and hereditary hemoglobinopathies for the autosomal recessive disorders, and myotonic dystrophy type 1, neurofibromatosis, Huntington’s disease, and hereditary cancer syndromes for the autosomal dominant disorders. For the X-linked disorders, PGT is mainly carried out for Duchenne’s muscular dystrophy, hemophilia A and B, and fragile X syndrome.. The specific disorders tested depend on the couple's genetic background and family history.
As there is more awareness among patients about the risks of transmitting genetic disorders and since the number of diseases with identifiable genetic cause(s) continues to rise, the total number of treatments as well as the list of indications for PGT is expected to expand in future.
Challenges of PGT-M
Despite its advantages, PGT-M presents several challenges. Developing a custom genetic test for each family can be technically demanding, especially for rare mutations or complex genetic backgrounds. The small amount of DNA obtained from the embryo biopsy requires highly sensitive and accurate testing methods. Amplification bias must be minimized, and potential contamination during biopsy carefully mitigated. Additionally, PGT-M is a specialized procedure and may require referral to specialized centers. It is also expensive and often not fully covered by insurance. Mosaicism, where some embryos have a mixture of cells with different genetic makeups, can complicate the interpretation of PGT-M results.
Future Advancements in PGT-M
Ongoing research and development are leading to exciting advancements in PGT-M. Non-invasive PGT-M (niPGT-M) is being explored, which involves analyzing cell-free DNA released by embryos into the culture media. This approach would eliminate the need for embryo biopsy, making the procedure less invasive and potentially more accessible. Improved sequencing technologies, including advances in NGS, enable more comprehensive and accurate genetic analysis of embryos, including the detection of multiple mutations and even whole-genome sequencing. Karyomapping is another promising technique that can be used for nearly all single gene disorders using linked SNP analysis. Unlike traditional methods, it does not require the creation of a patient-specific test.
Conclusion
PGT-M is a well-established tool that offers hope to couples at risk of passing on serious genetic disorders to their children. By enabling the selection of unaffected embryos, PGT-M can help break the cycle of inherited disease and allows families to make informed reproductive choices. While challenges remain in terms of technical complexity, cost, and ethical considerations, ongoing research and technological advancements promise to further enhance the accuracy, accessibility, and scope of PGT-M in the years to come. As our understanding of the human genome and gene editing technologies continues to grow, the potential of PGT-M to improve reproductive outcomes and reduce the burden of genetic disease is immense.
References:
- De Rycke, M. , & Berckmoes V. (2020). Preimplantation Genetic Testing for Monogenic Disorders. Genes, 11(8), 871. doi: 10.3390/genes11080871
- Chuva de Sousa Lopes, S. M., & Roelen, B. A. (2020). PGT in the era of advanced genetic technologies. Reproductive Biomedicine Online, 41(1), 1-10. doi:10.1016/j.rbmo.2020.04.011
- Harton, G. L., et al. (2021). Technological advancements in PGT: Current applications and future directions. Journal of Assisted Reproduction and Genetics, 38(3), 547-557. doi:10.1007/s10815-020-01978-4
- Zhang, H., et al. (2022). Non-invasive preimplantation genetic testing: Promises and challenges. Human Reproduction Update, 28(5), 754-766. doi:10.1093/humupd/dmac022
- Turocy, J. M., et al. (2023). The evolving landscape of PGT: Ethical and practical considerations. Fertility and Sterility, 120(2), 234-243. doi:10.1016/j.fertnstert.2023.04.004
- Liu, X. et al. (2024). Preimplantation genetic testing for monogenic disorders (PGT-M) for Monogenic nephropathy: a single-center retrospective cohort analysis. Clinical Kidney Journal,sfae356. Doi:10.1093/ckj/sfae356